Listen to this article
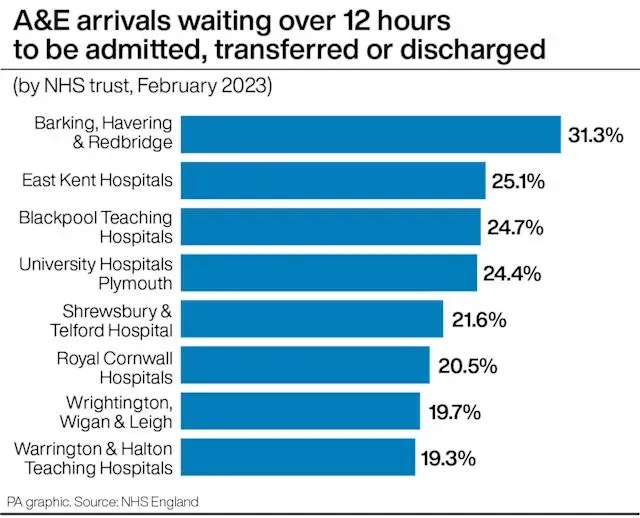
NHS A&E waiting times have reached alarming levels, with recent analysis highlighting that one in ten patients at major emergency departments in England spent over 12 hours awaiting treatment. Throughout 2025, a staggering 1.75 million patients faced such delays, illustrating the escalating pressure on NHS emergency services. Reports indicate a worrying trend of hospital waiting list UK, where patients are increasingly treated in corridors due to A&E treatment delays. The Royal College of Nursing has raised concerns about how these long waits are adversely affecting patient care in corridors, underlining a need for urgent reforms. As healthcare professionals advocate for improved conditions, the situation remains a critical issue that demands immediate attention from government officials and healthcare leaders alike.
In recent years, the challenges faced by England’s emergency services have escalated, particularly concerning NHS emergency department delays. The troubling statistic revealing that many individuals endure 12-hour A&E waits underscores the necessity for system reforms. As hospitals struggle with increased patient loads, the presence of patients receiving care in makeshift settings like corridors has become a significant concern. Moreover, the substantial hospital waiting list UK reflects the strain on healthcare resources amid rising treatment demands. It is imperative that stakeholders collaborate to address these urgent healthcare challenges to ensure dignity and safety in patient care.
Understanding NHS A&E Waiting Times
NHS A&E waiting times have become a crucial issue affecting patient care across England. In 2025, a staggering 1.75 million patients faced waits exceeding 12 hours at major A&E units, sparking widespread concern among healthcare professionals and organizations. This data emphasizes the urgent need to improve the efficiency of emergency services and ensure timely care for all patients attending these vital facilities. As patients wait for extended periods, not only is their health at risk, but the situation also puts immense pressure on the healthcare staff who are left to manage overcrowded environments.
The prolonged waiting times in A&E units can be attributed to numerous factors, including hospital emergency department delays that have been exacerbated over recent years. Despite the government’s acknowledgment of the unacceptable nature of these delays, the overall conditions in hospitals feel increasingly dire. For many, the experience of waiting in crowded conditions, sometimes treated in makeshift areas, contributes to a deteriorating sense of dignity and safety as delays spiral due to high patient volumes and insufficient staffing.
The Impact of Corridor Care on Patient Experience
Patients in NHS corridors are often subjected to discomfort and inadequate care while they wait for treatment. The practice of corridor care has been met with significant backlash from healthcare professionals, with several poignant testimonies illustrating the undignified conditions faced by patients. In various instances, patients have been treated in kitchen areas or dining rooms, raising serious concerns about patient privacy and safety. Disturbing accounts from nurses reveal that, in extreme situations, patients have tragically died while waiting unnoticed in these corridors, further exposing the severe impact of delayed care.
RCN members have expressed deep concern over the normalization of corridor care, illustrating the emotional toll it takes on healthcare providers who witness their patients suffering through undignified and unsafe conditions. With stories of elderly patients remaining forgotten in hallways for days, the importance of addressing these systemic issues becomes paramount. Health Secretary Wes Streeting’s commitment to eliminate corridor care by the end of the current parliament reflects a growing recognition that patient care must prioritize respect and dignity, fundamentally changing the current landscape of emergency services.
Hospital Waiting Lists and Their Implications
The context of NHS waiting lists adds layers of complexity to the issue of A&E waiting times. Currently, the waiting list in the UK for scheduled treatments, such as surgeries for knee and hip problems, continues to cause concern with approximately 7.31 million patients awaiting treatment. This figure represents a slight decline but still highlights the underlying issues of staffing shortages and resource allocation within the NHS, which affects not only planned patients but also those seeking emergency care and facing long waits in A&E.
As the government implements programs aimed at reducing waiting lists, the challenge remains in dealing with emergency department delays. The interaction between hospital waiting lists and A&E wait times presents a significant conundrum for healthcare officials trying to balance resources across different areas of patient care. Improvements in waiting lists have been noted, with significant reductions in waiting times seen in economically disadvantaged areas, but these measures must also translate into tangible benefits for patients faced with lengthy A&E wait times.
Challenges Faced by NHS Staff During A&E Waits
The relentless pressure on NHS staff has become a well-documented part of the narrative surrounding A&E waiting times. Those working on the front lines contend daily with the challenges of providing adequate care amidst overwhelming patient volumes and lengthy wait times. Reports from various A&E departments indicate a daunting struggle to maintain standards of care, especially when patients are treated in non-traditional settings like corridors or dining areas. Staff members often find themselves managing the emotional and physical turmoil of patients who are left to wait for treatments in unacceptable conditions.
Nurses and doctors report feeling demoralized as they navigate the fragmented healthcare system, where the urgency of patient care is often overshadowed by systemic inefficiencies. The commitment shown by these healthcare workers to provide the best possible care under difficult circumstances reflects a deep dedication to their practice. However, the ongoing pressures and delays can lead to burnout, calling into question the long-term sustainability of NHS workforce morale and effectiveness.
Government Response to NHS Emergency Department Delays
The UK government has publicly recognized the unacceptable nature of NHS emergency department delays, pledging to address this urgent issue moving forward. Health Secretary Wes Streeting’s commitment to transparency involves publishing detailed data on A&E waiting times and corridor care, emphasizing the administration’s intention to hold itself accountable in resolving these critical challenges. By shedding light on the extent of the waits faced by patients, the government aims to galvanize public support and resources towards effective solutions.
Despite the alarming statistics on A&E waiting times, there have been encouraging developments regarding ambulance response times, which the government reports have seen improvements in recent months. This highlights the dual nature of healthcare reform where, despite existing delays, some areas exhibit positive trends that can encourage further investment and resources that address not just A&E waiting times but improve overall patient care throughout the NHS.
Patient Accounts: The Human Cost of A&E Delays
Patient narratives surrounding A&E experiences showcase the profound human cost associated with extended waiting times. Accounts from individuals who had endured long waits in both corridors and chairs reveal feelings of confusion, fatigue, and anxiety about their well-being. One patient spoke of being left for hours without knowing what was happening, emphasizing that delays not only affect physical health but also take a toll on mental well-being. Such firsthand accounts underscore the significance of prioritizing timely and empathetic care within emergency departments.
Additionally, the lack of proper accommodations for waiting patients further compounds the distressing reality of A&E visits. From elderly individuals not being able to access comfortable seating to children witnessing troubling situations, these stories demonstrate how structural issues within the healthcare system can create unnecessary suffering. It is critical for healthcare leaders to listen to these voices and prioritize systemic changes that directly address the needs and voices of patients waiting in A&E.
Addressing the Future of NHS A&E Services
Moving forward, the future of NHS A&E services depends on the collaboration between government, healthcare professionals, and community stakeholders to devise effective strategies for managing patient flow and reducing waiting times. As the NHS grapples with the realities of growing patient numbers and resource constraints, innovative approaches must be adopted. This includes exploring alternative care models that prevent overcrowding in emergency departments and ensuring that patients can access the appropriate level of care in a timely manner.
Engaging frontline staff in the decision-making process is essential to implementing realistic solutions that can alleviate waiting times effectively. By investing in training, resources, and support for healthcare workers, the NHS can foster an environment conducive to improved patient outcomes. The potential to transform NHS A&E services lies in a collective effort to prioritize patient-centered care while addressing the systemic challenges that have plagued emergency services over the years.
The Role of Community Care in Reducing NHS A&E Pressure
Community care services play a vital role in alleviating pressure on NHS A&E departments by providing patients with alternatives for urgent care needs. Enhancing access to comprehensive primary care and outreach programs can significantly reduce unnecessary attendance at emergency services. Initiatives aimed at improving public health education about when to seek emergency care, along with investing in community-based health resources, can empower individuals to manage their health more effectively at home or with local providers.
Moreover, successful integration between community services and hospital systems can lead to streamlined patient care, reducing bottlenecks in A&E departments. By effectively managing local healthcare needs, the NHS can focus on providing timely care to those in genuine emergencies while preserving resources. The future of patient care hinges on a collaborative approach that emphasizes not just the treatment of illness but the overall management of health within the community.
Technological Innovations in NHS A&E Management
The integration of technology into NHS A&E management presents opportunities to optimize resource allocation and improve patient care delivery. Solutions such as real-time data tracking for patient flow can help identify bottlenecks in the system, allowing staff to make informed decisions to expedite care. Furthermore, advancements in telehealth services can facilitate remote triage, enabling patients to receive timely guidance on the appropriate level of care, which may prevent unnecessary A&E visits.
Additionally, utilizing electronic health records to assess patient histories and previous interactions with the NHS can streamline the treatment process upon arrival at A&E. By adopting a tech-first approach, NHS services can better handle patient volumes and ultimately reduce the stress placed on emergency departments, enhancing care quality and patient satisfaction. Embracing these innovations is critical in the ongoing effort to tackle NHS A&E waiting times and improve overall healthcare outcomes.
Frequently Asked Questions
What are the current NHS A&E waiting times like in 2025?
In 2025, approximately 10.1% of patients experienced waiting times of 12 hours or more at major NHS A&E units before being treated or admitted to a ward. This slight improvement from the previous year indicates ongoing challenges in managing NHS emergency department delays.
What impact do NHS A&E waiting times have on patient care?
NHS A&E waiting times significantly impact patient care, as many patients wait for hours in corridors, leading to unsafe and undignified treatment. Testimonies from healthcare professionals highlight concerns over patients receiving inadequate care in makeshift areas, emphasizing the urgent need for improvements in emergency services.
Why are patients facing 12-hour A&E waits at NHS hospitals?
Factors contributing to 12-hour A&E waits at NHS hospitals include staffing shortages, high patient volumes, and systemic challenges in the healthcare system. Despite some improvements noted this year, many hospitals still experience significant pressures that result in extended waiting times.
What is corridor care in the NHS, and why is it an issue?
Corridor care refers to the practice of treating patients in makeshift areas like corridors, which has become prevalent due to NHS A&E waiting times. This situation is problematic as it results in compromised patient dignity and safety, with healthcare providers expressing concern over the quality of care provided in such circumstances.
How does the NHS manage the hospital waiting list in the UK?
The NHS manages the hospital waiting list through targeted support programs aimed at counties with high rates of inactivity and by deploying specialist teams to improve efficiency. As of late 2024, there were approximately 7.31 million patients on waiting lists for planned hospital treatments, a figure that reflects ongoing efforts to reduce delays in the system.
What initiatives are being implemented to reduce NHS emergency department delays?
To address NHS emergency department delays, the government has committed to ending the practice of corridor care and improving transparency by publishing data on waiting times. Additionally, support programs for regions with high unemployment are being put into place to tackle the underlying issues contributing to delays.
What can patients do if they face long NHS A&E waits?
If patients encounter long NHS A&E waits, it is advisable to remain in communication with health staff for updates, understand their care options, and consider alternative services such as urgent care centers for less critical conditions. Awareness of their rights and available health resources can help patients navigate extended waiting times.
Are NHS A&E waiting times the same across the UK?
While NHS A&E waiting times vary slightly across the UK, all regions face challenges regarding emergency department delays. Each part measures waiting times differently, but trends indicate that most areas are struggling with similar issues impacting patient care and access to timely treatment.
What has been done to address the rising pressures on NHS emergency departments?
To alleviate rising pressures on NHS emergency departments, the government is focusing on improving staffing levels, increasing funding to support patient care, and reducing hospital waiting lists through enhanced operational efficiencies and resource allocations.
How has public perception of NHS A&E waiting times changed?
Public perception of NHS A&E waiting times has shifted as more attention is drawn to the issues of corridor care and patient safety. Concerns over long waits and substandard conditions have led to increased scrutiny of the NHS, prompting calls for urgent reforms to enhance patient care and experience.
| Key Point | Details |
|---|---|
| High 12-hour Waits | 1 in 10 major A&E patients waited over 12 hours for treatment in 2025. |
| Corridor Care Issues | Patients often have to wait in corridors or makeshift areas, leading to unsafe and undignified care. |
| Government Response | Health Secretary acknowledged unacceptable conditions and pledged to end corridor care and improve transparency. |
| Patient Experiences | Multiple testimonies reveal distressing experiences of patients waiting for long hours, often in uncomfortable conditions. |
| Waiting List Statistics | As of November, 7.31 million patients were on the waiting list for planned treatments; a slight decrease from the previous month. |
Summary
NHS A&E waiting times continue to raise significant concerns as analysis shows that one in ten patients spent over 12 hours waiting for treatment in major units. The statistics from 2025 indicate marginal improvement compared to the previous year, but issues such as corridor care remain serious points of contention. The Royal College of Nursing highlights the impact of long waits on patient dignity, providing harrowing accounts from healthcare professionals dealing with chaotic and inhumane conditions. The government admits the situation is unacceptable and commits to transparency and improvements, aiming to resolve corridor care practices. The focus must remain on providing quality care to patients, prioritizing their safety and dignity.