Listen to this article
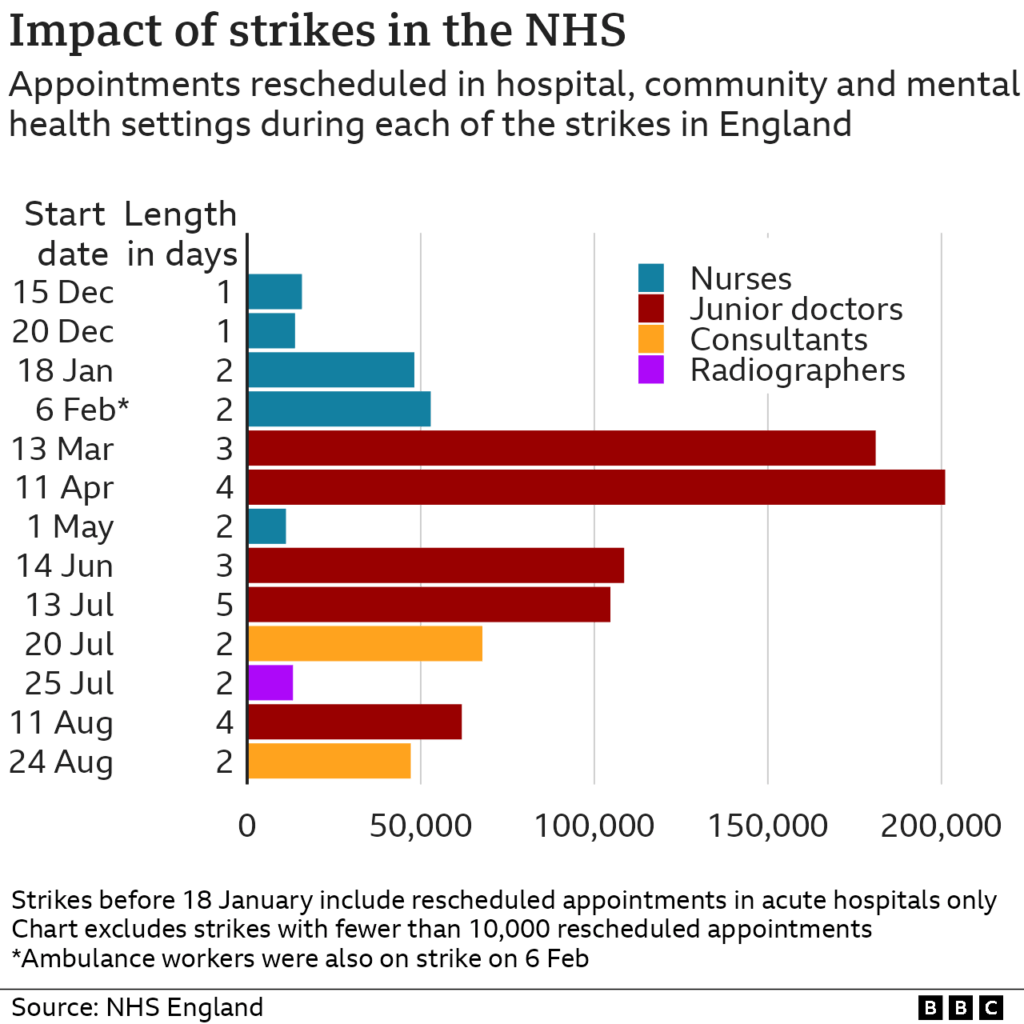
The ongoing doctor strike impact is resonating through the healthcare system, as health secretary Wes Streeting warns that this industrial action is causing significant distress for patients. With the latest round of strikes executed by junior doctors, also referred to as resident doctors, the implications for the NHS are dire, with many medical services facing interruptions. The British Medical Association (BMA) argues that low pay and insufficient training opportunities have driven the protests, urging the government to address the deep-seated issues plaguing the medical workforce. Streeting’s statements reveal a growing tension between healthcare providers and the government, emphasizing the urgent need for dialogue to alleviate the burdens on patients and the healthcare system. As the strike unfolds, the repercussions on patient care and access to medical services continue to mount, bringing the complexities of the NHS’s staffing crisis to the forefront of public discourse.
The implications of the ongoing industrial action among healthcare professionals extend beyond mere disruptions to schedules; they also reflect a broader crisis within the medical sector. The junior doctors’ protest encapsulates the frustrations surrounding inadequate compensation and a glaring shortage of available training positions. Amid the health secretary’s assertions, the strife among medical practitioners reveals a systemic challenge affecting the entire healthcare landscape. As the BMA navigates its demands, the focus must shift to a resolution that prioritizes both the welfare of healthcare workers and the essential needs of the community they serve. With every cancellation of appointments, the intimate connection between healthcare delivery and patient well-being becomes increasingly apparent.
The Consequences of the Doctor Strike on Patient Care
The ongoing doctor strike is deeply affecting the quality of care available to patients in England. Health Secretary Wes Streeting has publicly expressed concerns that the industrial action is ‘inflicting pain and misery’ on patients who rely on the NHS for their medical needs. As resident doctors participate in this five-day walkout, many patients face cancelled appointments and delays in critical medical evaluations. The implications of this strike are particularly troubling for those with urgent medical conditions, as they find themselves navigating a complicated system where care may not be readily available.
Hospitals, which rely heavily on resident doctors—who account for approximately half of the medical workforce—are experiencing increased strain. Even as the NHS attempts to maintain operations through other staff members and senior doctors stepping in, the efficiency of patient care is severely compromised. An example of this strain is highlighted by Chloe Rogers, a patient whose appointment was cancelled, leaving her health concerns unresolved. This situation illustrates not only the immediate impact on individual patients but also the broader implications for health outcomes across the NHS.
Impact of the BMA Strike on the Medical Workforce
The British Medical Association (BMA) strike highlights crucial conversations about the medical workforce in the UK. As junior doctors, now referred to as resident doctors, stand firm in their demands for better pay and training opportunities, the workforce faces critical shortages that threaten the sustainability of the NHS. The government’s inability to negotiate a satisfactory resolution with the BMA means that countless aspiring doctors could miss out on essential training positions, exacerbating the existing gaps in the medical workforce. This situation is particularly pressing as thousands of junior doctors vie for limited spots in residency programs each year.
Moreover, the health secretary’s statements criticizing the BMA’s actions as ‘morally reprehensible’ reflect a profound disconnect between the government and medical professionals. With the ongoing protests, the medical community is trying to advocate for a better working environment that not only ensures higher pay but also prioritizes patient care. As the BMA continues to press for enhancements in the recruitment and retention of doctors, the government must recognize the profound implications that such strikes have on the entire healthcare system.
Challenges Faced by Hospitals During the Strike
During the recent BMA strike, hospitals are grappling with significant operational challenges due to a reduced workforce. As Dr. Vicky Alner pointed out, while efforts are being made to keep patient care safe with the remaining medical staff, it has increased the workload and time taken to tend to patients. Typically, each ward would have multiple resident doctors, but with many participating in the strike, the burden falls heavily on senior consultants to manage patient care effectively. This inefficiency adds to the stress both for medical professionals and patients who may experience longer wait times for treatment.
Moreover, even though the NHS has made assurances that essential services will continue, the strain on hospitals raises concerns about the quality of care being provided. As noted in the experiences shared by patients whose appointments were cancelled, the ongoing dispute significantly affects individuals awaiting critical diagnoses and treatments. This situation illustrates the ripple effect of strikes on the healthcare system, as delays in care can lead to deteriorating health outcomes for patients that could have been preventable.
Public Sentiment Towards the NHS Doctor Strike
Public reaction to the NHS doctor strike is mixed, with many expressing sympathy for the resident doctors while also acknowledging the hardships faced by patients during this time. The plight of patients like Chloe Rogers, who have had appointments cancelled, draws attention to the detrimental consequences of the industrial action. Many observers understand that the doctors are fighting for fair pay and better working conditions, yet the impact on care delivery brings frustration and concern among the public who depend on these services.
There is, however, a growing discourse regarding the balance between the rights of medical professionals to organize and strike, against the pressing need for continuous patient care. While health officials advocate for improved compensation and working conditions for doctors, stakeholders in the healthcare system must work collaboratively to find solutions that honor those rights while ensuring patients receive timely and effective care. This ongoing tension reveals a crucial need for dialogue between the government, healthcare leaders, and medical professionals to navigate the complexities of wage disputes without sacrificing patient welfare.
Financial Implications of the Doctor Strike
The ongoing doctor strike is not just a healthcare issue—it has significant financial implications for the NHS and the broader economy. According to estimates, the strike could cost the NHS approximately £240 million, stemming from the need to cover for absent doctors and the potential loss of service delivery. This financial strain adds another layer of urgency to the negotiations between the BMA and the government as they try to resolve the pay disputes without additional disruptions to patient care.
Furthermore, the long-term financial repercussions of a strained healthcare workforce are profound. If the current disputes lead to fewer doctors entering training or remaining in the profession, the associated costs of recruiting and retaining qualified medical personnel could escalate. The government must recognize that providing fair wages and ensuring adequate working conditions for doctors not only supports the medical workforce but also serves the public interest in maintaining a functional, robust healthcare system.
Government’s Response to the Doctor Strike
In response to the ongoing BMA strike, the Health Secretary Wes Streeting has made several public statements addressing the issue. Streeting criticized the doctors’ actions, labeling them as reckless and detrimental to patient care. His remarks have stirred controversy within the medical community, as many doctors feel their legitimate concerns over pay and training opportunities are overshadowed by political rhetoric. The government’s current stance reveals a determination to maintain that a significant rise in salaries already occurred over the past few years, despite outward assertions from the BMA that pay continues to lag well behind inflation-adjusted figures from 2008.
This governmental perspective emphasizes the struggle that policymakers face: balancing budgetary constraints with the necessity for attracting and retaining qualified medical professionals. While Streeting has indicated that he is open to discussions on non-pay aspects, such as covering exam fees or increasing training placements, many doctors supplement these offers with the urgent clarification that without addressing their fundamental pay concerns, substantial progress cannot be achieved. The crux of the ongoing negotiations seems to rest on this underlying conflict between immediate financial constraints and the long-term health of the NHS.
The Role of Junior Doctors in the NHS
Junior doctors, or resident doctors, play a critical role within the NHS, serving as the backbone of many healthcare services across the country. Their extensive responsibilities include managing patient care, supporting senior consultants, and providing essential medical services, particularly in acute scenarios. The ongoing strikes spotlight the indispensable nature of their work while also highlighting their struggles over fair compensation and professional development opportunities amid a tough economic climate.
During this current dispute, junior doctors have voiced concerns not only about their salaries but also about the training infrastructure that is vital for upcoming medical professionals. As the BMA argues for better financial conditions and training placements, it reflects a growing awareness that investing in the training and well-being of junior doctors ultimately strengthens the entire NHS workforce. By addressing these necessities, the healthcare system can foster a more sustainable, capable, and motivated group of professionals dedicated to delivering high-quality patient care.
Future of Strikes and Negotiations in the NHS
The future of strikes and negotiations in the NHS hinges on the resolution of ongoing disputes between the government and medical representatives. As the BMA continues its push for improved pay and job security, the potential for further industrial action remains a significant concern. Without a proactive approach to negotiations, the NHS might face recurring disruptions that compromise patient care and hinder the overall functioning of the healthcare system.
Achieving a sustainable resolution requires a collaborative effort between the government, healthcare leaders, and doctors. Listening to the voices of those on the frontline, providing realistic and fair pay adjustments, and improving staffing levels in training positions could pave the way for a more harmonious relationship moving forward. Only through such negotiations will it be possible to address the tensions underlying the junior doctors’ protests and maintain the NHS’s integrity for future generations.
Community Reactions and Support for Striking Doctors
Community reactions towards the striking doctors often reflect a blend of frustration and solidarity. Patients recognize the dire implications of reduced services as appointments and surgeries are postponed, yet many express empathy towards the doctors’ plight for fair remuneration. The recent strikes have mobilized significant public interest and support, highlighting the necessity for equitable working conditions in a healthcare environment consistently under pressure.
In various communities, grassroots movements and public forums have emerged, allowing for discussion about the importance of supporting our medical workforce. As patients understand more about the challenges that doctors face, they often advocate for solutions that not only resolve the current disputes but also empower medical professionals to provide the best care possible. This collective support reflects a growing realization that enhancing physician conditions is integral to achieving positive health outcomes for the community at large.
Frequently Asked Questions
What is the impact of the NHS doctor strike on patient care?
The NHS doctor strike significantly impacts patient care, as expressed by Health Secretary Wes Streeting, who stated that the strike inflicts ‘pain and misery’ on patients. Essential services are strained, with hospital wards often staffing reduced numbers of doctors. Although NHS England aims to maintain most non-urgent operations, cancellations and delays in appointments have been reported, affecting patients’ health outcomes.
How are junior doctors protesting during the doctor strike and what do they demand?
Junior doctors, now referred to as resident doctors, are protesting through a five-day walkout, demanding better pay and more training opportunities. The British Medical Association (BMA) argues that pay remains significantly lower than its 2008 value when adjusted for inflation. The protests aim to draw attention to the need for a well-funded NHS that can adequately support its medical workforce and patient care.
What statements have been made by the Health Secretary regarding the doctor strike’s impact?
Health Secretary Wes Streeting has characterized the doctor strike as a reckless action that harms patients. He criticized the BMA for acting like a cartel and expressed frustration with the continued industrial action during a challenging time for the NHS, emphasizing the strain it puts on patient care and hospital operations.
What are the financial consequences of the BMA strike for the NHS?
The BMA strike incurs substantial financial consequences for the NHS, with estimates suggesting a cost of £240 million for the five-day walkout. This includes expenses related to staffing replacements and compensations associated with postponed medical services. The financial burden underscores the broader issue of funding and resources in the wake of ongoing strikes by healthcare professionals.
How is the medical workforce affected by the current junior doctors protest?
The current junior doctors protest heavily affects the medical workforce, with resident doctors constituting about half of the NHS’s medical personnel. The strike leads to increased reliance on consultants and senior doctors for patient care, while many resident doctors observe the strike. This situation not only impacts patient safety but also delays specialty training for many doctors entering the workforce.
Why is the junior doctors protest occurring now and what unresolved issues remain?
The junior doctors protest is occurring amid unresolved issues regarding pay and job availability. The BMA claims there is an impasse with the government, with resident doctors facing pay that is a fifth lower than it was in 2008, adjusted for inflation. Furthermore, there are significant concerns about insufficient training posts, which threaten the future supply of specialists within the NHS.
What proportion of NHS doctors are participating in the strike, and are any doctors still working?
Approximately two-thirds of resident doctors are participating in the current strike, as a significant portion are members of the BMA. However, about a third of resident doctors are not BMA members and will continue to work, thereby helping to mitigate the operational impact of the strike on patient services.
What has been the reaction of patients affected by the doctor strike?
Patients have expressed distress over the impact of the doctor strike, as many have faced cancellations of urgent appointments. For instance, Chloe Rogers, a patient from Nottingham, reported feeling ‘heartbroken’ after her urgent scan was cancelled, highlighting how the strikes directly affect the quality of life and healthcare outcomes for individuals in need of timely medical attention.
| Key Point | Details |
|---|---|
| Doctor Strike Consequences | Health Secretary Wes Streeting claims that the ongoing strike is inflicting pain and misery on patients. |
| Number of Striking Doctors | The current strike involves resident doctors (formerly junior doctors) in England, significantly affecting hospital operations. |
| Impact on Health Services | NHS aims to maintain 95% of non-urgent services by using available staff and offering overtime. |
| Economic Cost of Strikes | The NHS estimates the five-day strike could cost around £240 million. |
| Patient Experiences | Patients, like Chloe Rogers, report having urgent appointments canceled, significantly affecting their health. |
| Doctor’s Pay and Work Conditions | The British Medical Association (BMA) states that doctors’ pay is still a fifth lower than in 2008 after inflation adjustments. |
| BMA’s Position | The BMA emphasizes the need for more training places and fair pay, arguing that striking is a last resort. |
Summary
The doctor strike impact is significantly detrimental to the healthcare system and patients’ well-being. As the strike unfolds, it highlights critical issues in the NHS, including pay disparities and workforce shortages. Patients are feeling the brunt of the situation, with many experiencing canceled appointments and delays in care. It is essential that both the government and healthcare unions work collaboratively to resolve these disputes, ensuring that patient care remains a priority amidst the ongoing challenges faced by the NHS.