Listen to this article
Paracetamol overdose represents a critical healthcare challenge that can lead to severe consequences, including acute liver failure. In a tragic incident at Queen Elizabeth Hospital in London, a 55-year-old woman, Paula Doreen Hughes, succumbed to the effects of an accidental overdose of paracetamol, compounded by a medication error involving co-codamol. The oversight by medical staff in administering these drugs led to devastating outcomes, highlighting issues of hospital negligence and potential medical malpractice. This case serves as a stark reminder of the dangers associated with drug overdose and the necessity for vigilant medication management in healthcare settings. As more patients rely on over-the-counter medications and opioid combinations, the importance of preventing paracetamol overdose cannot be overstated.
The recent tragedy surrounding paracetamol overdose underscores the critical issue of administering safe medications in clinical environments. This incident raises significant concerns regarding prescription management and patient safety, particularly in instances of medical error and hospital shortcomings. When healthcare professionals overlook essential checks, such as duplicate prescriptions, patients risk severe outcomes, including fulminant liver damage. Moreover, this situation exacerbates the already pressing concerns related to systemic factors contributing to drug overdose incidents. It’s essential that healthcare establishments implement stringent protocols to prevent similar occurrences and safeguard patient welfare.
Understanding Paracetamol Overdose and Its Consequences
Paracetamol overdose is a serious medical condition that can lead to acute liver failure, one of the leading causes of mortality associated with drug overdoses. In the case of Paula Doreen Hughes, the hospital’s failure to adequately monitor her medication led to lethal consequences. Although paracetamol is commonly regarded as a safe over-the-counter medication, its safety margin is narrow, and exceeding the recommended dosage can have devastating effects on liver health. In this instance, the combination of prescribed co-codamol—another medication containing paracetamol—compounded the risk of overdose, illustrating the critical need for diligence in medication management.
The accidental overdose suffered by Mrs. Hughes underscores the pernicious nature of medication errors within hospital settings. When patients are prescribed multiple medications that contain overlapping active ingredients, such as paracetamol, the potential for acute liver failure increases dramatically. Medical professionals must always consider a patient’s complete medication history and current health status to avoid fatal mistakes. This incident serves as a stark reminder that drug overdoses can result from seemingly innocuous errors, emphasizing the importance of careful prescription practices.
The Role of Hospital Negligence in Drug Overdoses
Hospital negligence can significantly contribute to the risk of drug overdoses, as evidenced by the tragic case of Paula Doreen Hughes. Despite her clear symptoms of confusion, hospital staff failed to conduct proper assessments that could have revealed her history of medication use. The inquest identified several lapses in protocol, including the incorrect prescribing of multiple medications without checking for duplicates, a crucial step that could have prevented the overdose. This negligence raises critical questions about the accountability of healthcare providers and the systemic failures that contribute to such avoidable tragedies.
In situations like Mrs. Hughes’s, the implications of medical malpractice extend beyond individual practitioners. A lack of comprehensive training and inadequate systems for managing prescriptions can create environments where oversight and errors thrive. The recent coroner’s report highlights the need for systemic changes within healthcare facilities, including improved training for staff on medication management and patient evaluation. It is vital for hospitals to implement stringent checks—such as hard stops for duplicate prescriptions—to prevent similar cases of hospital negligence in the future.
Preventing Medication Errors in Healthcare Settings
To mitigate the risk of medication errors, healthcare facilities must adopt advanced technology and protocols that prioritize patient safety. One of the recommendations following the inquest into Paula Doreen Hughes’s death was the implementation of robust systems designed to flag duplicate prescriptions. By integrating automated checks into electronic health systems, medical staff can quickly identify potential medication conflicts and avoid unnecessary complications. Enhanced training on medication management for healthcare professionals is also critical to ensuring that they recognize the implications of prescribing practices.
Moreover, communication between healthcare providers and patients plays a vital role in preventing medication errors. Patients should be encouraged to disclose their complete medication history, including over-the-counter drugs, to avoid any interactions or overdoses. Training sessions that empower nursing and pharmacy staff to engage patients effectively can improve the accuracy of medication administration and reduce adverse drug events. As the healthcare community reflects on past mistakes, a renewed commitment to patient safety through better communication and technology adoption can greatly decrease the risk of medication errors.
Impacts of Drug Overdose on Patient Health
The consequences of a drug overdose, especially with medications like paracetamol, can be devastating not just for the individual but also for their families and the healthcare system at large. In Mrs. Hughes’s case, her overdose resulted in acute liver failure, necessitating intensive medical intervention and ultimately leading to her death. The profound impact of such incidents extends beyond the immediate medical complications; they also encompass psychological distress for loved ones who must navigate the aftermath of such tragedies. Understanding these consequences is crucial for both medical practitioners and families.
Furthermore, drug overdoses create significant strain on healthcare resources. The need for additional intensive care, longer hospital stays, and complex treatment plans can overwhelm medical systems already stretched thin. Each overdose incident compels healthcare practitioners to reassess their prescribing practices, communication strategies, and patient education initiatives. As healthcare providers work to reduce the incidence of drug overdoses, comprehensive strategies must include not only clinical improvements but also community education on the safe use of medications.
Legal Ramifications of Medical Malpractice in Overdose Cases
Medical malpractice cases arising from drug overdoses can lead to significant legal consequences for healthcare providers. In the unfortunate passing of Paula Doreen Hughes, the failures of multiple staff members in recognizing the signs of overdose and duplicative prescriptions raise questions about accountability and the ethical duties of care. Victims’ families may seek compensation for wrongful death, emphasizing the need for healthcare institutions to reinforce their commitment to patient safety with legal and financial repercussions for negligence. This underscores the critical role that regulations play in ensuring accountability within medical systems.
It is equally important for hospitals to establish transparent policies that address and rectify errors when they occur. This can include implementing disciplinary measures for those found negligent as well as creating a culture of openness where mistakes can be reported and learned from without fear of retribution. Such actions are not only necessary for patient safety but also essential for preserving the integrity of healthcare providers. Legal ramifications arising from cases of medical malpractice should serve as a catalyst for broader reforms in how healthcare institutions manage patient care and medication-prescribing protocols.
How Acute Liver Failure Affects Patients
Acute liver failure is a life-threatening condition that occurs when the liver suddenly loses its ability to function properly. This condition can be precipitated by drug overdoses, particularly those involving substances like paracetamol. For patients like Mrs. Hughes, acute liver failure can manifest through symptoms such as jaundice, confusion, and severe abdominal pain, ultimately leading to multi-organ failure without prompt medical intervention. Understanding the physiological effects and potential complications of liver failure is crucial for medical practitioners involved in the treatment of overdose cases.
Moreover, the psychological and emotional toll on patients experiencing acute liver failure can be profound. They may face long-term health complications, extensive medical treatments, and a complicated recovery journey. The unpredictability of the condition adds another layer of distress for patients and their families, often resulting in anxiety and fear regarding treatment outcomes. By fostering a comprehensive understanding of both the medical and emotional challenges faced by patients with acute liver failure, healthcare providers can offer more holistic care and targeted support to those affected by drug overdoses.
The Importance of Patient Communication in Medication Safety
Effective communication between healthcare providers and patients is vital in ensuring medication safety and preventing drug overdoses. In the tragic case of Paula Doreen Hughes, crucial information about her medication history was not effectively communicated to medical staff, which exacerbated her risk of receiving a duplicate prescription. Hospitals must develop protocols that prioritize open dialogue, encouraging patients to disclose all medications they are taking—including over-the-counter drugs—and any previous health issues. Such proactive communication can significantly mitigate errors like those that led to Mrs. Hughes’s death.
Furthermore, patients should be educated about the importance of asking questions and speaking up about their treatment plans. Empowering patients to take an active role in their healthcare can foster a collaborative approach that benefits both parties. Healthcare providers should initiate conversations that clarify potential side effects, interactions, and the significance of adhering to prescribed dosages. By prioritizing patient engagement and awareness, the healthcare system can work towards reducing the incidence of medication errors and enhancing overall patient safety.
Implementing System Changes for Future Safety
In light of the unfortunate case of Paula Doreen Hughes, it is imperative for healthcare institutions to implement systemic changes to prevent future medication errors and drug overdoses. Institutions like Lewisham and Greenwich NHS Trust have already begun proposing new strategies that include strict checks for duplicate prescriptions and improved training for staff on identifying patients’ medication histories. These changes are critical in creating a safer environment for patients and minimizing the risk of accidental overdoses in the hospital setting.
Beyond immediate solutions, healthcare systems must advocate for a culture that embraces continuous learning and quality improvement. This can be achieved through regular audits of prescribing practices, the integration of advanced technology for medication tracking, and ongoing education regarding the implications of drug overdose management. Comprehensive strategies that focus on systemic improvements will not only honor the memory of victims like Mrs. Hughes but will also actively contribute to the prevention of similar tragedies in the future.
The Future of Drug Safety: Lessons Learned from Medical Errors
The tragic case of Paula Doreen Hughes serves as a poignant reminder of the need for ongoing efforts to improve drug safety within healthcare. Lessons learned from such medical errors can be transformative if they are used to inform changes in patient care protocols and clinical practices. Continuous monitoring and evaluation of prescribing patterns, as well as fostering a culture of accountability, are key components of a healthcare system committed to patient safety.
As the medical community adapts to new challenges, embracing innovations like electronic health records and decision-support systems can help to prevent similar occurrences in the future. These technologies can assist providers in avoiding medication errors that lead to drug overdoses, ensuring that patients receive safe and appropriate treatments. Ultimately, the goal is to create a clinical environment where patient safety is the top priority, informed by the hard-earned lessons of past mistakes.
Frequently Asked Questions
What are the dangers of paracetamol overdose?
Paracetamol overdose can lead to severe liver damage, acute liver failure, and even death. When taken in excessive amounts, the liver becomes overwhelmed and cannot process the drug safely, which can cause toxic by-products that harm liver cells.
How can hospital negligence contribute to paracetamol overdose?
Hospital negligence can significantly contribute to paracetamol overdose through errors such as failing to check for duplicate prescriptions or not accurately assessing a patient’s medication history. This negligence can lead to patients inadvertently receiving excessive doses of paracetamol, as seen in the tragic case of Paula Doreen Hughes.
What should I do if I suspect a paracetamol overdose?
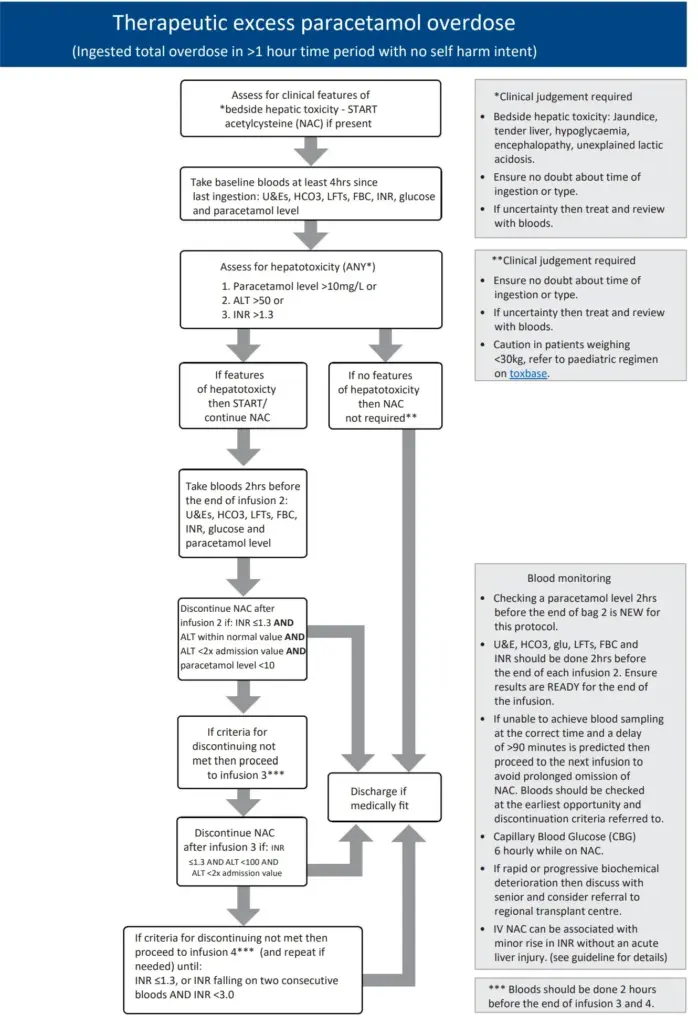
If you suspect a paracetamol overdose, seek immediate medical attention. Time is critical, and healthcare professionals can administer treatments like n-acetylcysteine, which can help prevent or mitigate liver damage if given early enough.
What are common causes of medication error leading to paracetamol overdose?
Common causes of medication errors that may lead to paracetamol overdose include miscommunication among healthcare providers, lack of patient medication history, and inadequate systems for monitoring prescription duplicates. Training and awareness among medical staff are essential to avoid such errors.
How is acute liver failure related to paracetamol overdose?
Acute liver failure is often a result of paracetamol overdose because the liver is the primary organ that metabolizes this medication. When taken in high doses, paracetamol can produce toxic metabolites that damage liver cells, leading to rapid and severe liver failure.
What role does medical malpractice play in cases of paracetamol overdose?
Medical malpractice may play a significant role in paracetamol overdose cases when healthcare providers fail to meet the standard of care, such as neglecting proper patient assessments, resulting in inappropriate prescriptions that cause drug overdoses.
What preventive measures can hospitals take to avoid paracetamol overdose?
Hospitals can implement several preventive measures against paracetamol overdose, including robust systems to check for duplicate prescriptions, staff training on medication safety, and improved communication protocols to ensure comprehensive patient medication reviews.
What are the symptoms of paracetamol overdose?
Symptoms of paracetamol overdose can initially be vague and may include nausea, vomiting, loss of appetite, confusion, and abdominal pain. These symptoms can progress to jaundice, liver failure, and coma if not treated promptly.
Can paracetamol overdose be treated successfully?
Yes, paracetamol overdose can be treated successfully if recognized early. The administration of the antidote n-acetylcysteine can significantly reduce the risk of liver damage if given within 8 to 10 hours post-ingestion.
How often does drug overdose occur in hospitals?
Drug overdose in hospitals can occur more frequently than expected, often due to human error, prescribing mistakes, or miscommunication among healthcare staff. Rigorous safety protocols are necessary to minimize such incidents.
| Key Points | Details |
|---|---|
| Accidental Overdose | Paula Doreen Hughes, a 55-year-old woman, died after being given an overdose of paracetamol and co-codamol at Queen Elizabeth Hospital in London. |
| Date of Incident | January 6 to January 8, 2022: Mrs. Hughes was prescribed both paracetamol and co-codamol repeatedly. |
| Cause of Death | Liver failure due to paracetamol overdose led to her passing on January 9, 2022. |
| Hospital Errors | Multiple medical staff failed to recognize the duplicate prescription, leading to a delay in treatment. |
| Coroner’s Inquest | Coroner Liliane Field noted negligence from doctors, nurses, and pharmacists, highlighting a need for better systems. |
| NHS Response | The NHS Trust announced new protocols to prevent such incidents from recurring, including training and prescription checks. |
Summary
Paracetamol overdose is a serious medical issue, as highlighted by the tragic case of Paula Doreen Hughes, who died following an accidental overdose at a London hospital. Despite multiple prescriptions for paracetamol, hospital staff failed to recognize the danger posed by duplicate medications. The incident underscores the critical need for healthcare providers to ensure accurate medication management and enhance communication regarding a patient’s medication history. In light of this tragedy, the NHS is implementing new protocols designed to prevent future occurrences of paracetamol overdose and improve patient safety.