Listen to this article
Maternal deaths remain a pressing concern, as a recent study highlights the alarming trend of avoidable fatalities among pregnant women and new mothers in hospitals. Despite coroner recommendations aimed at preventing maternal deaths, significant gaps in hospital care for mothers continue to persist. Between 2013 and 2023, over 29 cases of maternal deaths were reported, primarily occurring in healthcare settings during or shortly after childbirth. The study reveals troubling factors such as hemorrhages, mental health crises, and inadequate medical attention, emphasizing the critical need for maternity care improvements. Without timely interventions and systemic changes, the journey to safeguarding maternal health remains fraught with challenges that demand urgent attention.
Addressing the alarming issue of maternal fatalities, or the deaths of women due to complications related to pregnancy and childbirth, highlights a systematic failure in healthcare responses. Various studies spotlight the need for enhancing maternity services and ensuring comprehensive hospital care for mothers before, during, and after delivery. The implications of coroner findings serve as crucial recommendations that call for immediate action in order to prevent future tragedies. Additionally, the importance of postpartum mental health cannot be overstated, as deteriorating psychological well-being after childbirth often exacerbates the risks. By focusing on these critical aspects, we can improve outcomes and effectively tackle the troubling rates of maternal deaths.
The Importance of Addressing Maternal Deaths in Healthcare
Maternal deaths represent a grievous indication of a healthcare system’s effectiveness, particularly in maternity care. The recent study by Kings College London highlighted that gaps in hospital care are leading to preventable tragedies. In England and Wales, nearly one-third of the reported maternal deaths were attributed to lapses in appropriate treatment, underscoring the urgent need for healthcare providers to implement recommended coroner advice to improve safety. This commitment to addressing maternal deaths is crucial not only for the health of mothers but also for the well-being of families and future generations.
In recognizing and responding to the alarming maternal death rates, healthcare institutions must prioritize systemic changes backed by evidence. As per the coroner’s recommendations, timely escalation of care and improvements in staff training are necessary steps toward preventing future incidents. The study’s findings serve as a call to action for policymakers and hospital administrators to recognize maternal deaths as pivotal indicators of care quality, prompting robust maternity care improvements that can save lives.
Understanding the Role of Coroner Recommendations
Coroner recommendations play a vital role in shaping healthcare practices concerning maternal care. Their insights draw attention to systemic failures within hospitals that may otherwise go unnoticed. The findings from Kings College London’s analysis indicate that a staggering number of maternal deaths stemmed from inadequacies in care, such as the failure to provide timely medical intervention. By heeding the advice from coroners, healthcare organizations can address these deficiencies, reinforcing their commitment to prioritizing maternal health.
Moreover, when organizations act upon coroner recommendations, they not only enhance the quality of care for mothers but also create actionable frameworks for staff training and policies. The data shows that when PFDs were acknowledged, 80% of organizations reported implementing changes that could directly impact postpartum care and mental health. This connection highlights a critical loop of accountability where coroner recommendations become catalysts for meaningful transformation in maternity services.
Enhancing Hospital Care for Mothers
Improving hospital care for mothers is essential in preventing maternal deaths, as highlighted in recent studies. Implementation of thorough training for healthcare staff, alongside adherence to recommendations from coroners, can significantly mitigate the risks associated with childbirth. According to the PFD reports, many maternal deaths could have been avoided with better care protocols and quicker response times to complications such as hemorrhaging, which was noted in nearly 27% of cases. Hospitals must adopt a proactive stance on maternal health by prioritizing comprehensive training and education for their medical personnel.
Additionally, hospitals should leverage technology and data analytics to monitor maternal health outcomes continuously. This approach allows for the identification of trends that may indicate areas requiring immediate attention. Collaborative efforts among healthcare practitioners and researchers are crucial to develop and sustain improvements in maternity care systems. By ensuring that hospitals adhere strictly to coroner recommendations and cultivate a culture of accountability, the likelihood of maternal deaths can be dramatically decreased.
The Impact of Postpartum Mental Health
Postpartum mental health issues, such as postpartum depression and psychosis, are critical factors that can lead to tragic outcomes if left unaddressed. The case of Alex Baish illustrates just how detrimental a lack of appropriate mental health support can be, highlighting the need for hospitals to provide comprehensive postpartum care. Mental health screenings during postpartum visits should be reinforced, ensuring that mothers who exhibit symptoms receive immediate and adequate support. Failure to recognize these signs can have devastating impacts on families and communities.
Implementing structured mental health programs within maternity care can serve to reduce stigma and provide mothers with the support they need to cope during a pivotal time in their lives. By prioritizing postpartum mental health, healthcare providers will not only prevent potential tragedies but also foster healthier family dynamics. The acknowledgment of mental health as a critical component of maternal care must be woven into the fabric of maternity services to ensure that every mother feels supported and safe during the postpartum period.
Maternity Care Improvements and Their Necessity
Maternity care improvements are vital for ensuring the health and safety of mothers and newborns alike. The research conducted by Kings College London underscores that proactive responses to coroner reports are essential. Hospitals need to identify systemic weaknesses and initiate changes that align with best practices for maternity care. Commitment from healthcare organizations to enhance maternity services not only leads to better outcomes for mothers but also safeguards the next generation.
Furthermore, continuous evaluation and adaptation of maternity care protocols are necessary to keep pace with evolving medical guidelines and research findings. The focus should expand beyond reactive measures to encompass a culture of excellence in maternal health care. Investing in training, resources, and support systems for healthcare staff will enable them to better recognize and respond to the needs of mothers during and after childbirth, ultimately contributing to a more robust healthcare framework.
The Role of Families in Maternal Health Advocacy
Families play a crucial role in advocating for better maternal health care, as evidenced by emotional accounts such as Richard Baish’s advocacy following his wife’s untimely demise. The support system that families provide can often help mothers navigate the complexities of postpartum care and mental health. Raising awareness around maternal health issues and sharing personal experiences can catalyze necessary changes in health systems, ensuring that women’s voices are heard and addressed.
Furthermore, families can seek to educate themselves and others about the signs of postpartum complications and the available resources for mental health support. Engaging in dialogues with healthcare providers about concerns regarding maternal care can empower families to advocate for systemic changes that improve safety and care quality. By fostering a community-oriented approach toward maternal health, families can contribute to decreasing maternal deaths and enhancing the experience for new mothers.
The Importance of Timely Response in Maternal Care
Timely responses in maternal care are one of the critical components that can prevent unnecessary fatalities. The findings from the coroner reports indicate that delays in escalations of care significantly contribute to adverse outcomes for women during childbirth and postpartum. Hospitals must implement protocols that ensure swift action when complications arise, thereby minimizing the risks associated with maternal health emergencies. Continuous training on recognizing critical signs among hospital staff is crucial for improving response times.
Moreover, healthcare systems should prioritize establishing clear communication channels among staff to relay critical maternal health information effectively. Teams should have structured protocols for responding to maternal emergencies, which include mental health crises. By fostering a culture of urgency and preparedness, hospitals can make significant strides toward reducing maternal deaths and ensuring a safer environment for mothers and their babies.
The Need for Data-Driven Decision Making
Data-driven decision-making is essential in enhancing maternal health care quality and preventing future deaths. By analyzing prevention of future deaths reports comprehensively, healthcare providers can identify patterns, gaps, and areas needing improvement. The current maternal death rates and corresponding circumstances documented in the reports should be used as benchmarks for evaluating the efficacy of implemented recommendations. Organizations that actively engage in data analysis are better equipped to make informed decisions concerning training, resource allocation, and protocol updates in maternity care.
Additionally, ongoing research and collaboration with institutions like Kings College London can help sustain a continuous feedback loop where data fuels policy reform and operational improvements. With evidence-based decisions being the cornerstone of effective healthcare, maternity services can adapt dynamically to emerging challenges. This proactive approach ensures that maternal health remains a focused priority, ultimately mitigating risks and enhancing outcomes for mothers and babies.
Coronial Inquest Findings and Their Implications
The findings from coronial inquests are vital sources of information that highlight systemic failures in maternity care, prompting necessary changes within healthcare institutions. By closely reviewing these inquests, healthcare providers can gain insight into the causes of maternal deaths and the contributing factors that need attention. Such scrutiny is crucial, as it often reveals trends that may not be immediately visible to practitioners in their daily operations. Public awareness and institutional responsiveness to coronial findings can engender an environment where maternal pulse detection is prioritized.
Additionally, incorporating coronial inquest findings into broader educational programs for medical and nursing staff can promote a culture of learning and improvement. Ensuring that all staff members understand the severe implications of inadequate maternal care is fundamental to transforming hospital environments. When the systematic recommendations from inquests are actively followed, healthcare facilities can significantly improve safety protocols and foster confidence among expectant mothers in the services provided to them.
Frequently Asked Questions
What measures are being taken to prevent maternal deaths during hospital care?
Preventing maternal deaths in hospital care requires integrating prevention of future deaths (PFDs) reports into maternity practices. This includes implementing new local policies, enhancing staff training, and ensuring timely escalation of care for complications, particularly during and after childbirth.
How do coroner recommendations help in reducing maternal deaths?
Coroner recommendations play a crucial role in addressing systemic issues that lead to maternal deaths. They identify gaps in care, such as mismanagement of complications and inadequate training of staff, which, when addressed, can significantly reduce maternal mortality rates.
What are the common causes of maternal deaths identified in recent studies?
Recent studies have identified that hemorrhage accounts for 27% of maternal deaths, while suicide is a significant concern, claiming the lives of 20% of women. Additionally, complications during early pregnancy, such as ectopic pregnancies or terminations, have also been highlighted as contributing factors.
How can maternity care improvements impact postpartum mental health?
Maternity care improvements, including proper screening and support for mental health during the postpartum period, are essential for preventing maternal deaths. By addressing mental health proactively, such as recognizing signs of postpartum psychosis early, healthcare providers can ensure that new mothers receive the urgent help they need.
Why is it critical to monitor trends in maternal deaths?
Monitoring trends in maternal deaths is vital to identify recurring issues and inform necessary changes in care practices. By systematically addressing gaps identified in PFD reports, healthcare systems can proactively implement strategies to prevent future tragedies and improve overall maternal health outcomes.
What can families do to advocate for better maternity care to prevent maternal deaths?
Families can advocate for better maternity care by remaining informed about the signs of postpartum complications and being proactive in communicating concerns to healthcare providers. Awareness of coroner recommendations and supporting the implementation of new health policies can also contribute to systemic improvements in maternity care.
How frequently do maternal deaths occur in England, and what is being done to address this?
The maternal death rate in England for 2021/23 was reported at 12.82 per 100,000 births. This alarming rate has prompted calls for urgent action, including the integration of coroner recommendations into public health strategies, to ensure that healthcare practices are aligned with the latest findings to prevent maternal deaths.
What role does staff training play in preventing maternal deaths in hospitals?
Staff training is vital in preventing maternal deaths as it ensures that healthcare professionals are equipped with the latest knowledge and skills to manage complications effectively. Improved training can lead to better identification of high-risk cases and prompt action, addressing the major causes of maternal fatalities.
| Key Points |
|---|
| Research shows that hospitals are ignoring coroner advice to prevent maternal deaths. |
| A study identified 29 maternal deaths between 2013 and 2023, primarily occurring in hospitals and after childbirth. |
| Hemorrhage is the leading cause of maternal death, with 27% of cases. |
| 20% of maternal deaths were due to suicide, showing a mental health crisis among new mothers. |
| Coroners highlighted failures in treatment and care escalation in over 48% of reports. |
| Only 38% of Prevention of Future Deaths (PFD) reports received responses, although 80% of responding organizations made changes. |
| Dr. Georgia Richards emphasized the need for monitoring and systematic actions to improve maternal care. |
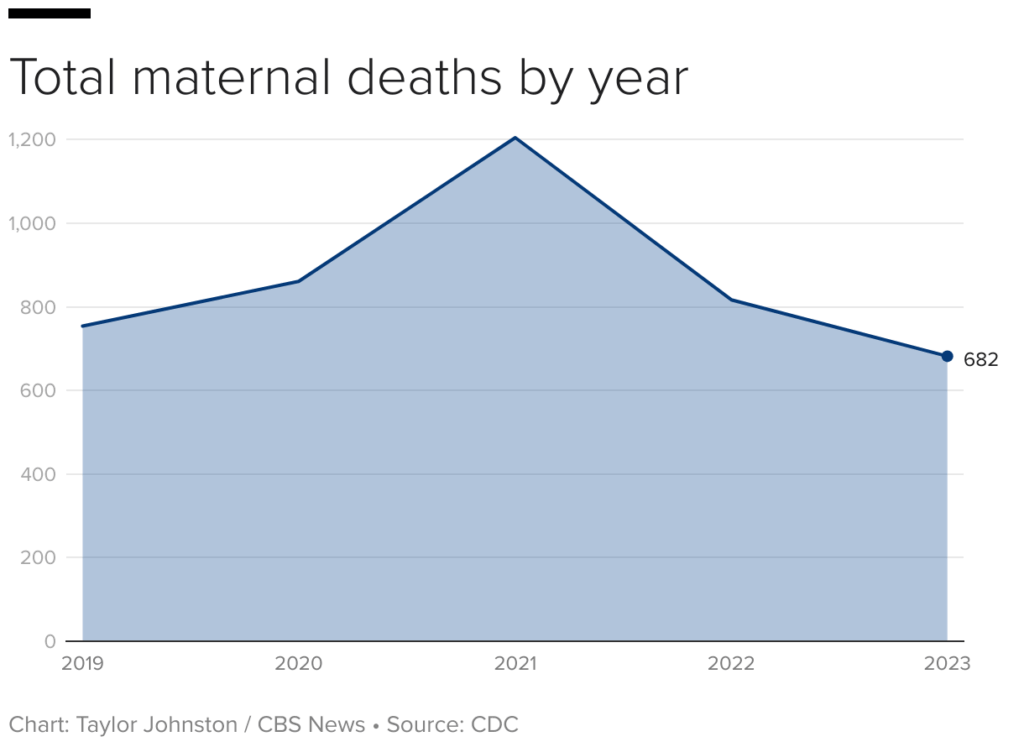
| The maternal death rate in England was 12.82 per 100,000 births for the period 2021-2023. |
| Urgent actions are needed to ensure that the concerns of mothers and pregnant individuals are prioritized. |
Summary
Maternal deaths remain a significant concern in today’s healthcare system. The recent findings from Kings College London expose alarming gaps in care and highlight the urgent need for change within maternity services. With a maternal death rate of 12.82 per 100,000 births in England, it is crucial to address the systemic failures that leave mothers vulnerable, particularly regarding mental health and timely medical treatment. Continued efforts to monitor and act on coroner recommendations will be essential in preventing future tragedies and ensuring the safety of mothers and their newborns.