Listen to this article
NHS waiting times have become a pressing concern for patients and healthcare providers alike, particularly as nearly a quarter of hospitals in England have reported increased delays since the government’s efforts to tackle the NHS backlog were implemented. The rise in hospital waiting times has raised alarms, highlighting significant healthcare delays that impact patient care across various regions. Many individuals, like the elderly Mary Waterhouse, are left suffering from worsening conditions due to the slow pace of receiving necessary treatments, such as knee and hip surgeries. These struggles underline the importance of meeting NHS treatment targets, as patients await essential care amid typically rising patient numbers. As the government reiterates its commitment to improving services, striving for timely interventions remains a critical issue for the UK’s healthcare system.
Hospital waiting periods have recently emerged as a significant topic of discussion, revealing the ongoing challenges faced by patients seeking timely medical attention. The noticeable increase in delays across numerous healthcare facilities reflects a broader issue within the NHS, where long-standing treatment backlogs continue to hinder effective patient care. The urgency to address these healthcare setbacks grows as hospitals navigate various barriers, including staffing shortages and outdated systems. Individuals enduring extended waits for essential services, such as surgical procedures, are increasingly vocal about their experiences, emphasizing the need for urgent reforms. As the healthcare landscape evolves, addressing these pressing matters will be paramount to ensuring equitable access to care for all.
The Deteriorating NHS Waiting Times: A National Concern
Recent analyses reveal a troubling trend in NHS waiting times for hospitals across England, with nearly a quarter reporting worsened conditions since a government plan to tackle healthcare delays was introduced. This situation underscores a significant concern as hospitals are struggling to maintain the NHS treatment targets, particularly the critical 18-week waiting timeframe for essential procedures such as knee and hip surgeries. The government has set ambitious goals to alleviate the NHS backlog, but many hospitals face challenges in staffing, technology issues, and logistical hurdles that complicate their ability to meet these standards.
Patients like Mary Waterhouse have become emblematic of this crisis, often enduring excessive waiting times that significantly impact their quality of life. Reports show that despite a national effort to reduce NHS waiting times, individual experiences can vary drastically, with some regions facing more severe backlogs. This disparity highlights the need for targeted interventions to ensure equitable access to patient care across all NHS trusts, sparking conversations about the overarching sustainability of the healthcare system in England.
Factors Contributing to NHS Backlog and Healthcare Delays
The NHS backlog and increasing waiting times are influenced by various interconnected issues that need urgent addressing. Staffing shortages have been identified as one of the primary reasons leading to delays in treatment. Hospitals have reported an escalation in doctor strikes and an increasing demand for prioritized care in complex cases, which diverts attention and resources away from routine treatments. This multifaceted problem is exacerbated by the introduction of new IT systems, as seen in Epsom and St Helier NHS trusts, where disruptions have delayed patient processing and care delivery.
Moreover, the variability in performance among NHS trusts indicates that while some are making progress, others are seeing minimal improvements or even declines in their ability to meet waiting time targets. This inconsistency suggests systemic inequalities that impact patient access and care quality differently across regions. Advocacy groups like Healthwatch England have called for heightened oversight to monitor the most affected trusts, pushing for accountability and performance improvement strategies that can bridge these patient care gaps.
The Impact of Patient Experience on NHS Waiting Lists
The experience of patients waiting for care not only reflects the pressures on healthcare systems but also highlights the personal struggles faced during lengthy delays. Many patients, like Mary, report a significant decline in their health and well-being while waiting for treatment. These experiences are more than just statistics; they encapsulate the emotional and physical toll that prolonged waiting times can impose. Timely interventions are crucial, as delayed treatments can lead to deteriorating health conditions, further complicating diagnoses and resulting in the need for more extensive procedures.
In addition to physical ailments, long waiting times contribute to increased anxiety and emotional distress among patients, potentially leading to a cycle of health deterioration. The importance of timely healthcare cannot be overstated, as prompt treatment can lead to better outcomes and enhance life quality. Advocates highlight the need for practices that acknowledge patient experiences, urging NHS management to prioritize timely interventions to mitigate the impact of healthcare delays on lives.
Anticipated Changes in NHS Waiting Time Guidelines
As the government prioritizes reducing NHS wait times, several key guidelines are being discussed to ensure progress towards achieving the 18-week treatment target by March 2029. One approach focuses on investing in surgical hubs and expanding service availability through evening and weekend appointments. These initiatives aim to alleviate pressure on hospitals, optimize staff utilization, and ultimately enhance patient flow, making timely care more accessible.
However, successfully implementing these changes will take concerted effort from all stakeholders involved, from healthcare administrators to frontline staff. The unique challenges faced by various NHS trusts indicate that a one-size-fits-all solution may not be suitable. Overall, continuous evaluation of these guidelines and their impact is vital in shaping future healthcare policies, ensuring that they remain responsive to patients’ needs and capable of addressing long-standing issues in the NHS.
Comparison of NHS Treatment Targets Across Regions
There is marked variability in how different NHS trusts perform against treatment targets, indicating significant disparities in access to timely care across the regions. The target of 92% of patients being treated within 18 weeks may have been set at the national level, but its consistency and implications vary widely depending on local conditions and challenges. For instance, trusts in more deprived areas face higher levels of demand and systemic weaknesses, leading to greater difficulties in meeting these targets. Areas with significant healthcare disparities often struggle more with NHS backlogs, underscoring the need for tailored solutions.
Encouragingly, some trusts have demonstrated that substantial improvements are feasible. By learning from these successful cases, the NHS can implement best practices and strategies to uplift poorer performing trusts. Comparative analysis can also provide insights for healthcare planners, allowing them to identify areas in need of additional resources and specific interventions to enhance patient care experience.
Strategies for Addressing NHS Hospital Waiting Times
Mitigating NHS hospital waiting times requires a multi-faceted approach encompassing policy reform, healthcare funding, and innovative solutions. Currently, the government’s strategy includes establishing targeted funding for underperforming NHS trusts. This is intended to facilitate their recovery and meeting established thresholds for patient care. Additionally, the integration of technology and improved data systems can streamline management tasks, allowing healthcare professionals to allocate time more effectively and prioritize patient care where it is needed most.
Moreover, fostering collaboration amongst hospitals and community healthcare can enhance efficiency in patient management. By creating seamless referral pathways and shared resources, the burden on individual trusts may be lightened, facilitating a more holistic approach to patient treatment. Implementing such strategies not only addresses waiting times but also improves overall service delivery and patient satisfaction across the healthcare spectrum.
Patient Advocacy in the NHS: A Call for Action
Patient advocacy remains a cornerstone of efforts to reform the NHS and address the persistent issue of waiting times. Organizations such as Arthritis UK emphasize the critical role of patient voices in shaping healthcare policies and ensuring that the individual experiences of those affected by waiting times inform institutional strategies. Advocates argue that focusing on the human element of healthcare – the struggles, pain, and resilience of individuals – is essential for creating effective solutions.
Furthermore, involving patients in decision-making processes can provide valuable insights into the realities of waiting times and treatment accessibility. This collaborative approach not only empowers patients but also promotes a culture within the NHS where patient care is prioritized, potentially leading to improved resources and more comprehensive solutions to combating NHS treatment delays.
Future Outlook for NHS Waiting Times and Treatment
Looking ahead, the future of NHS waiting times depends on the continued commitment to reform and resource allocation aimed at alleviating backlogs. With ongoing monitoring and accountability measures in place, there is hope for significant improvements in patient care experiences, provided that trust-specific challenges are addressed. The planned enhancements in service availability, as well as the expansion of treatment facilities, could signal a positive shift towards meeting NHS waiting targets and improving overall healthcare delivery.
It is essential, however, to acknowledge that the factors influencing waiting times extend beyond immediate fiscal considerations. Systemic issues such as healthcare equity, workforce management, and operational efficiencies must be continuously evaluated to ensure sustainable progress. As the NHS works toward achieving its ambitious goals, maintaining transparency and engaging with patients will remain critical components in fostering trust and improving the delivery of care.
Frequently Asked Questions
What are the current NHS waiting times for hospital treatments?
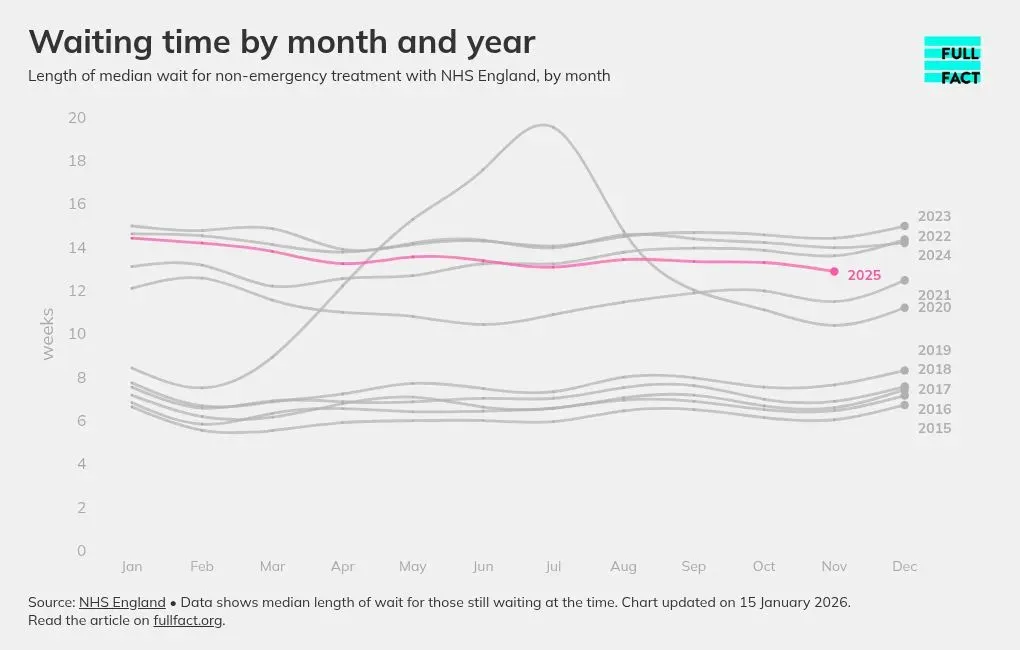
NHS waiting times for hospital treatments currently vary significantly across the country. As of the latest data, while the overall waiting list has decreased to 7.31 million patients, specific hospitals are facing severe delays. The government aims to ensure that 92% of patients are seen within 18 weeks; however, nearly a quarter of hospitals reported worsening waiting times recently.
How does the NHS backlog affect patient care?
The NHS backlog has a direct impact on patient care, resulting in long waiting times for essential treatments. Many patients face significant delays, which can worsen their health conditions. For instance, patients with arthritis, like Mary Waterhouse, have reported waits of up to eight months, leading to severe consequences for their overall well-being.
What measures are being taken to address NHS treatment targets?
To tackle NHS treatment targets, the government has committed to meeting the 18-week waiting time by March 2029, with an interim target of 65% by March 2026. Investments are being made in services, including new surgical hubs, to improve efficiency and reduce waiting times across NHS trusts.
Why are some hospitals experiencing longer NHS waiting times?
Some hospitals are experiencing longer NHS waiting times due to various challenges, including staffing shortages, strikes by healthcare professionals, and IT system disruptions. These factors have led to regressions in meeting treatment targets, particularly in trusts that already faced operational difficulties.
What should patients do if they are facing long NHS waiting times?
Patients facing long NHS waiting times should communicate with their healthcare provider about their concerns and options. It may also be beneficial to seek advice from patient advocacy groups like Healthwatch England, which can provide support and guidance on navigating the NHS system effectively.
Are there any recent trends in NHS hospital waiting times?
Recent trends indicate mixed progress in NHS hospital waiting times; while some trusts have improved, others have reported significant declines. For example, a few trusts have improved their waiting times by substantial margins, while others, like East Cheshire, have seen a notable decrease in patients waiting under 18 weeks.
How does the NHS measure waiting times for treatments?
The NHS measures waiting times for treatments based on the duration patients wait from the point of referral to the start of treatment. The target is that 92% of patients should be treated within 18 weeks, and progress towards this target is monitored regularly, though local performance can vary significantly.
What impact do staffing shortages have on NHS waiting times?
Staffing shortages have a considerable impact on NHS waiting times, as inadequate staffing can lead to delays in treatment and care. This has been highlighted by various NHS trusts, where increased patient demands and prioritization of urgent cases, such as cancer referrals, have exacerbated waiting periods for planned treatments.
How are healthcare delays being addressed within the NHS?
Healthcare delays are being addressed by the NHS through targeted funding, improved resource allocation, and strategic initiatives such as extending service hours during evenings and weekends. These efforts aim to enhance patient throughput and ultimately reduce waiting times for treatments.
What is the significance of the NHS waiting times target?
The NHS waiting times target is significant because it sets a benchmark for patient care, ensuring that a high percentage of patients receive timely treatment. This target aims to reduce the backlog and promote equitable access to health services, which is essential for improving overall health outcomes.
| Hospital Trust | Change in Patients Waiting < 18 Weeks (%) | Key Issues Faced |
|---|---|---|
| East Cheshire | -10% | Staff shortages, IT issues. |
| Barnsley | -9% | Increased cancer referrals, staff shortages. |
| Whittington Health | -5% | General operational issues. |
| Epsom and St Helier | -5% | New patient record system disrupting services. |
| Shrewsbury and Telford | +17% (Improvement) | Significant operational improvements implemented. |
Summary
NHS waiting times remain a critical issue, with nearly a quarter of hospitals in England experiencing worsening levels since the government’s plans were announced. Despite some hospitals showing improvements, many are still falling behind in meeting the vital 18-week waiting target. Patients are enduring longer wait times due to various factors, including staffing shortages and IT disruptions. Addressing these challenges will be essential to ensure patients receive timely treatments, ultimately improving the overall healthcare experience in the NHS.