Listen to this article
NHS hospital discharge delays are becoming a pressing issue across the UK, as hospitals struggle to free up beds for incoming patients. Currently, thousands of individuals remain in hospital care long after their treatment has concluded, leading to increased hospital bed occupancy rates and significant financial strains on the NHS. Delayed discharges are not only causing logistical challenges for healthcare providers, but they also leave patients in hospital unnecessarily, potentially exacerbating their health issues. The root causes of these delays often stem from NHS funding issues and difficulties in securing timely care home placements for vulnerable elderly patients. As the healthcare system grapples with these challenges, the need for an effective strategy to streamline the discharge process has never been more critical.
The ongoing challenges surrounding patient exits from NHS facilities highlight significant hurdles in the healthcare system, commonly referred to as discharge obstacles. Many individuals awaiting transfer to appropriate care settings are often stuck in hospital wards, intensifying the strain on hospital resources and resulting in reduced availability for new admissions. As the demand for beds escalates, factors such as budgetary constraints and the complexities of arranging proper social care become increasingly evident. The situation is compounded by a reliance on insufficient community care options and a lack of coordination between various healthcare entities. Addressing these discharge bottlenecks is essential to ensure that patients receive care environments suitable to their needs, while simultaneously enhancing operational efficiency within the NHS.
Understanding NHS Hospital Discharge Delays
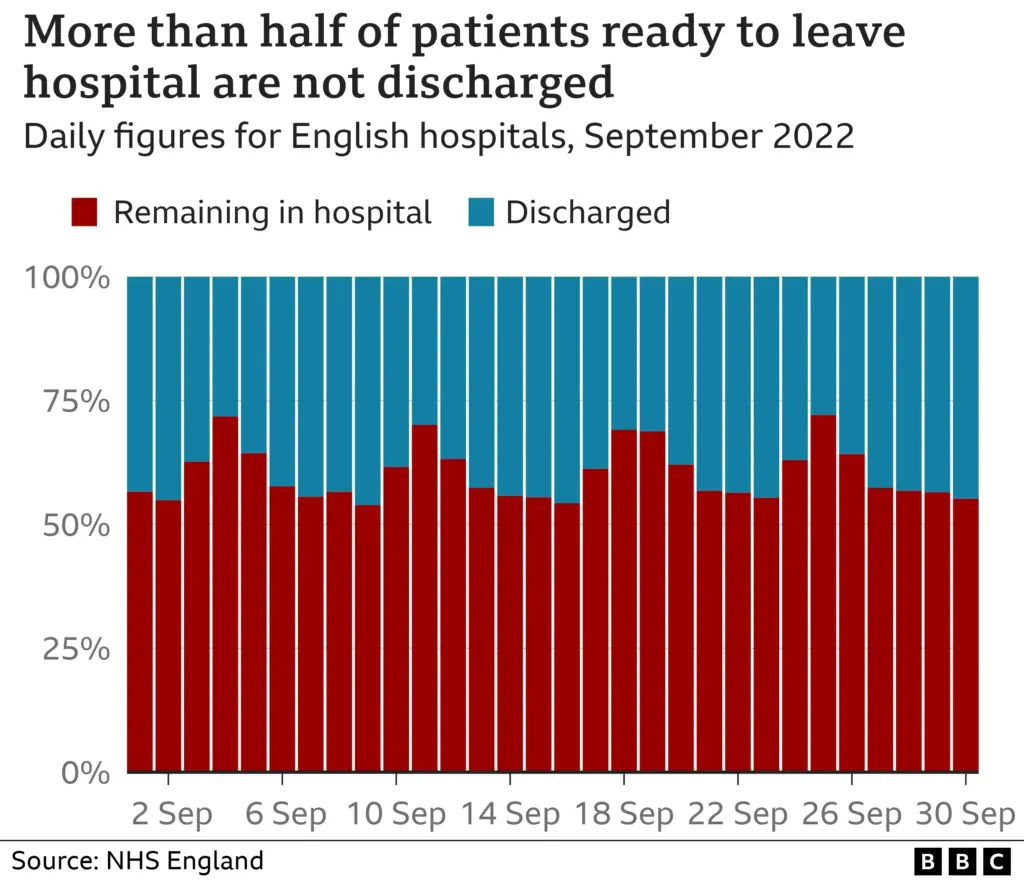
NHS hospital discharge delays have reached a critical level, with thousands of patients remaining in hospitals long after their treatment is complete. Reports indicate that over 13,000 patients in England are occupying beds that could be freed up for those who need immediate medical care. These delays not only strain hospital resources but also lead to increased healthcare costs, with each occupied bed costing the NHS over £500 a day. This situation reflects a widespread inefficiency that compromises patient care across the healthcare system.
Given that nearly one in eight NHS beds is taken up by patients who should be discharged, it’s essential to understand the myriad factors contributing to these delays. The involvement of local authority-run social care services is critical. Patients often require home adaptations, nursing support, or even placements in care homes, but bureaucratic delays and insufficient funding for social services can prolong their stay in hospitals drastically.
The Financial Impact of Delayed Discharges
The financial implications of delayed discharges in the NHS are staggering, with estimates suggesting a loss of over £225 million each month due to unnecessary bed occupancy. This affects not just the financial health of the NHS but also the overall quality of care other patients receive. The delays lead to cancelled surgeries and extended emergency department waits, as hospitals struggle to manage patient inflow while simultaneously housing individuals who no longer need acute medical care.
Moreover, the costs extend beyond hospital budgets, impacting social care systems as well. Local councils, burdened by tight budgets and rising demand, often find themselves unable to provide the necessary support for timely patient discharges. The pressure on healthcare budgets exacerbates funding issues within NHS facilities, resulting in incapacitated services struggling to offer timely care.
The Role of Social Care in Hospital Discharges
Social care plays a fundamental role in facilitating timely hospital discharges. In several successful models, social workers coordinate with healthcare professionals to prepare for discharge as soon as patients are admitted. This proactive approach is critical to minimizing delays and ensuring patients transition safely back into their homes or suitable care environments. However, cooperation between health and social care sectors is often inconsistent, leading to fragmented services that can hinder effective discharge planning.
For instance, initiatives across the UK illustrate that when NHS teams and local authorities collaborate closely, discharge rates improve significantly. This collaboration is exemplified at Queen Elizabeth Hospital in Gateshead, where a discharge liaison hub collaborates with social services to ensure quick and well-coordinated patient transitions. Such models highlight the necessity of combining resources and expertise to alleviate the strains of delayed discharges.
Exploring Alternative Solutions to Reduce Delayed Discharges
To combat delayed discharges, some NHS trusts are exploring alternative solutions, such as creating dedicated ‘step-down’ facilities where patients can recover without occupying hospital beds. These facilities, which resemble intermediate care beds, not only relieve pressure on hospital wards but also provide essential supportive care in a less acute environment. For example, projects like the former care home in Leicester demonstrate the potential effectiveness of investing in such facilities, successfully allowing patients to leave hospitals while maintaining access to essential healthcare services.
Countries like Denmark have demonstrated that integrated healthcare services, including community nursing and rehabilitation programs, can drastically reduce the dependency on hospital care. By investing in these alternatives, the NHS could free up valuable resources, ensuring that patients in need of acute care receive the attention they require while simultaneously addressing the issue of delayed discharges.
Challenging Family Perspectives on Hospital Care
Family dynamics complicate the issue of hospital discharge. Many families believe that keeping their relatives in the hospital is the safest option, stemming from a perception that hospitals offer better protection against medical crises. However, this belief may inadvertently contribute to the cycle of delayed discharges, as families may resist or delay discussions about transitioning their loved ones to community care or home settings.
Healthcare professionals often find themselves navigating these sensitive conversations, educating families on the risks that extended hospital stays pose, such as increased frailty and reduced independence. Emphasizing the benefits of home or community-based care can help shift these perspectives and encourage quicker discharges, demonstrating that hospitals are not always the ideal environment for recovery for those no longer in need of acute medical intervention.
End-of-Life Care and the Need for Reform
The question of how end-of-life care is managed within the NHS is also central to the dilemmas surrounding hospital discharges. Many patients nearing the end of life find themselves admitted to hospitals and subjected to unnecessary interventions and prolonged hospital stays, which can worsen their quality of life. As healthcare professionals reassess their approach to treating these patients, prioritizing palliative care can enhance patient satisfaction and outcomes, ensuring that those at the end of life receive compassionate care in a suitable setting.
To address these challenges, healthcare systems must recognize the importance of appropriate care transitions from acute settings to more suitable environments. By increasing investments in palliative care services and integrating them into the standard care process, institutions can reduce the pressure on hospitals while ensuring that patients receive the dignity and care they deserve as they approach end-of-life scenarios.
Improving Integration Between NHS and Social Care
The integration of NHS services with local social care is vital in addressing the issue of delayed discharges effectively. Many patients struggle with a lack of community support, prompting prolonged stays in hospitals due to unavailable care home placements or insufficient in-home assistance. Enhancing the relationship between the NHS and social care providers ensures that patients can transition smoothly and swiftly to their homes or care facilities, preventing unnecessary bed occupancy.
Reports highlight that improved cooperation can lead to a five-fold decrease in delayed discharges. This success underscores the need for strategic partnerships, whereby healthcare professionals align with social workers to devise comprehensive discharge plans. When healthcare systems prioritize such collaboration, they are better positioned to address the challenges posed by delayed discharges, ultimately benefitting the entire healthcare system.
The Impact of NHS Funding Issues on Patient Care
Ongoing NHS funding issues play a pivotal role in exacerbating the challenges of delayed discharges. Financial constraints faced by both healthcare facilities and local authorities hinder their ability to deliver timely and sufficient care. Underfunded social care systems often struggle to recruit staff or enhance services needed for safe and timely discharges, creating a bottleneck that extends beyond individual hospitals.
As local councils confront rising demand and cost pressures, it becomes increasingly difficult to maintain adequate services, thus impacting patient flow within NHS institutions. Addressing these funding issues is crucial for the future of patient care, as improving financial investment in both NHS and social services would enable better coordination and ultimately less reliance on hospital resources for patients who should be receiving care elsewhere.
Learning from International Models of Care
Looking internationally, the UK’s NHS can learn from how other healthcare systems manage patient transitions effectively. For example, countries like Denmark have implemented integrated healthcare services that promote quick and efficient transitions from hospitals to community care settings. These models focus on preventative care, effective home support, and intermediate care options that keep patients out of acute care environments unless necessary.
By adopting similar strategies, the NHS could see a significant reduction in delayed discharges and a transformation of patient care dynamics. Investment in community-based services, enhanced care positions, and streamlined discharge processes can foster a more adaptable healthcare system, ultimately benefiting patients.
Frequently Asked Questions
What are the main causes of NHS hospital discharge delays?
NHS hospital discharge delays are primarily caused by a lack of available care home placements, inadequate community care resources, and persistent NHS funding issues. These delays can result in patients occupying hospital beds unnecessarily, leading to increased hospital bed occupancy and compromising care for other patients.
How can delayed discharge impact NHS hospital bed occupancy?
Delayed discharge significantly contributes to NHS hospital bed occupancy, with approximately one in eight beds occupied by patients ready for discharge. This situation exacerbates pressures on the NHS, leading to canceled surgeries and prolonged wait times in emergency departments as hospitals struggle to accommodate new patients.
What are the financial implications of delayed discharge in the NHS?
Each day, maintaining a hospital bed costs the NHS around £562, which means that delayed discharge can lead to more than £225 million in losses monthly. This financial strain affects the overall resources of health services, limiting their ability to provide timely care for patients genuinely in need.
Are elderly patients a major factor in delayed discharge within the NHS?
Yes, many elderly patients, often living with multiple health conditions, contribute to NHS delayed discharges. These patients frequently require post-discharge support, such as home care or rehabilitation services, complicating their timely exit from hospitals.
What role do care home placements play in NHS hospital discharge delays?
Care home placements are crucial for alleviating NHS hospital discharge delays. Many patients ready for discharge cannot leave the hospital until appropriate placements are available. The lack of such placements often leads to increased bed occupancy and extended hospitalization for patients who no longer need acute medical care.
What strategies has the NHS implemented to address hospital discharge delays?
The NHS has initiated several strategies to tackle hospital discharge delays, including improving cooperation between social care and the NHS, establishing discharge liaison hubs, and creating additional care home facilities to provide necessary support for patients after they leave hospital care.
How do NHS funding issues exacerbate hospital discharge delays?
NHS funding issues exacerbate hospital discharge delays by limiting the resources available for social care services, which are essential for facilitating timely discharges. Insufficient funding leads to resource constraints in providing community-based support, forcing many patients to remain in hospital longer than necessary.
What innovative practices can improve NHS hospital discharge processes?
Innovative practices, such as implementing integrated discharge hubs that involve social workers and medical staff, can greatly improve NHS hospital discharge processes. Early discharge planning and effective communication between care services also play critical roles in ensuring patients transition smoothly to post-hospital care.
How does public perception affect NHS hospital discharge delays?
Public perception can significantly affect NHS hospital discharge delays. Families often prefer hospital settings for their loved ones due to perceived safety, even when home care may be more beneficial. This preference can delay necessary discharges and complicate the care process.
What are the potential solutions to reduce delayed discharges in the NHS?
Potential solutions to reduce delayed discharges in the NHS include enhancing funding for social care, improving coordination between healthcare providers, developing more intermediate care facilities, and increasing public education on the benefits of timely discharges and care at home.
| Key Point | Details |
|---|---|
| NHS Hospital Discharge Delays | Over 13,000 patients in England occupy hospital beds unnecessarily after treatment, contributing to bed shortages. |
| Financial Implications | Each hospital bed costs approximately £562 per day, leading to over £225 million wasted monthly in England. |
| Impact on Patient Care | Delayed discharges result in cancelled surgeries and increased wait times in Emergency Departments. |
| Profiles of Delayed Patients | Patients often include elderly individuals needing extensive community support. |
| Need for System Reform | Collaboration between NHS and social services is vital to address the discharge delays. |
| Good Practices | Successful models include integrated discharge hubs in some hospitals that expedite patient transitions. |
| International Examples | Countries like Denmark implement structured intermediate care to avoid hospital stays with community-based support. |
| Family Dynamics | Family reluctance to engage in caregiving leads to patients remaining in hospitals longer than necessary. |
| End-of-Life Care Challenges | Hospitals can sometimes over-treat patients nearing the end of life, complicating discharge efforts. |
Summary
NHS hospital discharge delays continue to plague the healthcare system, leading to unnecessary financial strain and adverse patient outcomes. With thousands of patients remaining in hospital beds after treatment is completed, it is clear that addressing this issue is critical for improving care coordination, reducing costs, and enhancing the overall patient experience. Effective strategies and collaboration between the NHS and social care services remain vital to resolve these delays.