Listen to this article
Hospital falls are a critical concern in inpatient safety, significantly impacting patient care and recovery. Each year, thousands of patients experience unwitnessed falls in healthcare settings, often leading to serious injuries or even fatalities, such as head injury risks that can snowball into dire consequences. The recent tragedies at St George’s Hospital in south London underscore the alarming reality of overstretched resources and NHS staffing issues that contribute to such incidents. Without adequate nursing supervision, vulnerable patients like David Ward and Dr. Debapriya Ghosh can suffer grievously due to a lack of appropriate care and risk assessments. It is imperative that hospitals prioritize hospital safety to mitigate these risks, enhance supervision protocols, and ensure that every individual receives the necessary support during their stay.
Patient accidents in medical facilities, particularly falls, represent a pressing issue that affects many healthcare institutions. Incidents where individuals slip or tumble without witnesses, often during critical recovery periods, highlight the dangers that arise in environments where resources are strained. The alarming cases from St George’s Hospital demonstrate how systemic NHS staffing issues can exacerbate these situations, leading to conditions where adequate nursing supervision is compromised. Such occurrences not only jeopardize patient safety but also illustrate the need for comprehensive evaluations and increased vigilance in monitoring at-risk patients. By addressing these challenges, hospitals can significantly reduce the incidence of unwitnessed falls and promote a safer healing environment.
Understanding Hospital Falls and Their Impact on Patient Safety
Hospital falls represent a critical issue in patient care, especially in overstretched healthcare systems. The recent incidents at St George’s Hospital, where two patients died following unwitnessed falls, highlight the urgent need for improved nursing supervision and comprehensive risk assessments. According to reports, both men suffered head injuries due to lack of adequate support and monitoring from nursing staff, underlining the significant consequences that can arise when hospitals fail to adhere to established safety protocols.
Patient safety must be a top priority for healthcare facilities, as falls in hospitals can lead to severe injuries, prolonged recoveries, and in tragic cases, death. Implementing rigorous fall prevention strategies, such as enhanced nursing oversight and regular safety audits, is essential in mitigating risks associated with patient falls. The correlation between hospital staffing issues and the high rate of falls cannot be overstated; as demand for services increases, the strain on available resources often results in lapses in care that jeopardize patient safety.
The Role of Nursing Supervision in Preventing Patient Falls
Nursing supervision plays a vital role in preventing hospital falls, particularly for vulnerable patients. As illustrated by the inquests into the deaths of David Ward and Dr. Debapriya Ghosh, the absence of continuous monitoring and appropriate risk assessments can lead to catastrophic outcomes. Effective nursing care entails not only attending to immediate medical needs but also proactively managing potential fall risks through vigilant supervision and timely interventions.
Enhanced nursing supervision can significantly reduce the incidence of falls in hospitals. Hospitals should implement training programs that emphasize the importance of risk assessment and patient monitoring, particularly for patients exhibiting signs of frailty or confusion. By adopting a proactive stance, nursing teams can identify patients at risk for falls and take preventive measures to ensure their safety, ultimately improving the overall patient care experience within healthcare facilities.
Head Injury Risks Associated with Hospital Falls
Head injuries resulting from falls in hospitals pose serious health risks, often leading to long-term complications or fatalities. With the recent tragedies at St George’s Hospital, both men suffered severe head injuries due to their falls, reinforcing the critical nature of thorough risk assessments and preventive protocols. Patients admitted with preexisting conditions, such as confusion, infection, or frailty, are particularly susceptible to falls and require vigilant care.
Effective communication and collaboration among healthcare providers are essential in mitigating head injury risks. When specific patient needs are overlooked due to high demands on staff, as seen in the cases of Ward and Ghosh, the likelihood of falls and resulting injuries increases significantly. Addressing hospital safety can reduce head injury risks and improve recovery outcomes, emphasizing the importance of prioritizing patient monitoring and individualized care plans.
Examining NHS Staffing Issues and Their Effect on Patient Care
NHS staffing issues have become a focal point in discussions about patient care and safety in hospitals. The tragic deaths at St George’s underscore how significant staffing shortages can adversely impact patient outcomes. With caregivers stretched thin, it is increasingly challenging to provide the level of supervisory care required, especially for those at higher risk for falls or requiring immediate attention.
An overstretched workforce can lead to burnout and job dissatisfaction among healthcare professionals, further exacerbating staffing challenges. Hospitals must recognize the importance of addressing staffing issues not only to enhance patient safety but to support their nursing staff effectively. Initiatives to recruit and retain qualified personnel must be prioritized to ensure that patients receive the attentive care necessary to reduce the risk of falls and improve overall well-being.
Implementing Changes to Improve Hospital Safety Post-Incidents
In the wake of the recent falls at St George’s Hospital, immediate changes have been proposed to bolster hospital safety and prevent similar incidents in the future. By increasing staffing levels and implementing comprehensive falls assessments, hospitals can better address patient needs and ensure appropriate care is provided in a timely manner. These changes are crucial for improving patient outcomes and restoring trust in healthcare systems.
Moreover, hospitals should conduct regular quality and safety rounds to monitor compliance with safety protocols actively. Creating a culture of safety within healthcare settings requires ongoing commitment from all levels of staff to be vigilant about patient care and proactive in preventing incidents. By focusing on continuous improvement and accountability, healthcare facilities can significantly reduce the incidence of falls and enhance the overall quality of patient care.
The Importance of Family Involvement in Patient Care
Family involvement is a crucial aspect of patient care, particularly in environments where nursing staff may be overwhelmed. In the cases of Ward and Ghosh, their families provided essential support during their hospital stays but ultimately could not prevent the falls that led to tragic outcomes. Encouraging family members to participate in the care process can enhance patient safety, as they can alert staff to potential risks based on their intimate knowledge of the patient’s condition.
Healthcare facilities should facilitate open communication with families, ensuring they understand their role in patient safety and care. This collaboration enhances the continuity of care and allows for better risk assessments, especially when patients face cognitive challenges. By integrating family members into the care team, hospitals can create a more supportive environment for patients, ultimately contributing to better health outcomes and fewer incidents of falls.
Developing Comprehensive Fall Prevention Programs
Developing comprehensive fall prevention programs is integral to improving hospital safety and protecting patients. Such programs should include tailored risk assessments, staff training on fall prevention strategies, and frequent evaluations of patient care practices. The tragic incidents at St George’s Hospital highlight the need for a proactive approach to fall prevention, emphasizing the importance of continuous staff education and awareness.
Effective fall prevention programs must also involve multidisciplinary teamwork, where nurses, physicians, and support staff collaborate to create and implement safety protocols. Regularly reviewing these protocols in light of recent incidents can help identify gaps in care and ensure that all personnel are equipped to provide high-quality care. Through rigorous training and collaboration, hospitals can drastically reduce the incidence of falls and improve patient safety outcomes.
The Consequences of Onward Care Post-Discharge
The consequences of inadequate care post-discharge can have lasting effects on patient health and safety, particularly for those returning home after significant hospital incidents. Without proper follow-up care and safety measures, patients may be at increased risk for falls and other complications following discharge. The tragic losses of Ward and Ghosh highlight the critical need for a robust transition plan that encompasses follow-up care and resources to prevent further incidents.
Hospitals must ensure that patients and their families are equipped with clear discharge plans, which include information on managing health conditions, recognizing risks, and accessing community support services. Coordinating care with outpatient providers can bridge the gap between hospitalization and safe recovery at home. By prioritizing continuity of care, hospitals can significantly mitigate the risks associated with post-discharge complications, enhancing patient safety and overall health outcomes.
The Future of Patient Safety in Overstretched Healthcare Systems
The future of patient safety in overstretched healthcare systems depends on the ability to adapt and reform in light of increasing demands. The incidents at St George’s Hospital serve as a powerful reminder of the need for systemic changes in how patient care is delivered, particularly in high-pressure environments like emergency departments. By prioritizing staffing enhancements, streamlined patient management protocols, and rigorous safety assessments, healthcare systems can create safer environments for patients.
As hospitals move forward, the emphasis must be on cultivating a culture of safety where every staff member understands their role in preventing patient falls and safeguarding health outcomes. Investing in ongoing education, technology advancements, and collaborative safety efforts can revolutionize hospital care delivery. By doing so, healthcare institutions can better manage demand, reduce risks, and ultimately improve the quality of care afforded to every patient, ensuring that tragedies like those at St George’s Hospital become increasingly rare.
Frequently Asked Questions
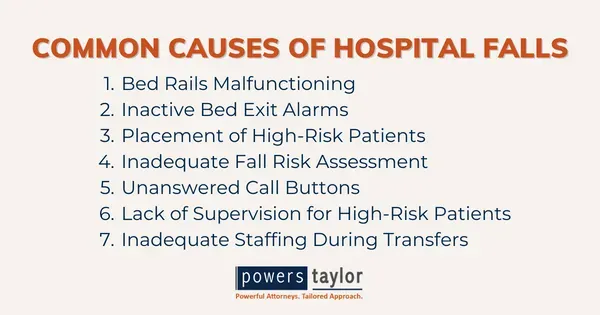
What are the common causes of hospital falls related to patient care?
Hospital falls can occur due to various reasons, including inadequate nursing supervision, slippery floors, patients being in unfamiliar settings, and underlying medical conditions like frailty or delirium. Ensuring thorough patient assessments for fall risk is essential for preventing these incidents.
How can nursing supervision reduce the risk of hospital falls?
Effective nursing supervision is crucial in mitigating fall risks. Nurses can monitor patients with increased fall risk closely, conduct regular assessments, and provide timely assistance, ensuring patients have the necessary support to prevent falls, particularly during critical recovery periods.
What measures can hospitals implement to improve safety and prevent falls?
To enhance hospital safety and reduce fall incidents, hospitals can increase staffing levels, conduct comprehensive risk assessments for all patients, implement regular safety rounds, and provide specialized care for at-risk patients, such as one-to-one nursing when necessary.
Why are head injury risks significant in hospital fall incidents?
Head injuries from falls in hospitals are particularly concerning because they can lead to severe complications or death, especially in elderly or frail patients. Proper nursing supervision and timely interventions can help minimize these risks significantly.
What role do NHS staffing issues play in preventing hospital falls?
NHS staffing issues directly impact the level of patient care and supervision, which are pivotal in preventing hospital falls. Overworked and understaffed facilities may struggle to provide adequate monitoring and support, increasing the likelihood of incidents.
How can families help prevent unwitnessed falls in hospitals?
Families can play a crucial role in minimizing the risk of unwitnessed falls by remaining vigilant about their loved one’s condition, communicating any concerns to the staff, and ensuring that their family members receive the necessary assistance before leaving their side.
What changes have hospitals made to improve patient care and reduce fall incidents following recent tragedies?
In response to past incidents, hospitals have implemented immediate changes such as increasing staffing levels, conducting comprehensive fall risk assessments, expanding emergency care units, and ensuring that frail patients receive enhanced care, which collectively aim to better prevent future falls.
How does effective patient care influence the rates of hospital falls?
Effective patient care, characterized by proactive assessments, adequate supervision, and timely interventions, is vital in reducing the rates of hospital falls. Continuous improvements in care practices and proper staffing can lead to significantly safer hospital environments.
What impact do falls have on hospital safety measures?
Falls significantly undermine hospital safety measures, influencing protocols, staffing decisions, and overall patient care strategies. Each incident typically leads to deeper investigation and reforms aimed at enhancing patient safety and preventing recurrence.
What should patients and families know about hospital safety concerning falls?
Patients and families should be aware of the risks associated with hospital stays, advocate for proper assessments, and remain engaged with healthcare providers to ensure that appropriate measures are in place to minimize the risk of falls during their hospital care.
| Key Point | Details |
|---|---|
| Hospital Context | St George’s Hospital in Tooting, south London, is currently overstretched, impacting patient care. |
| Victims | David Ward, 76, died on 10 February 2024; Dr. Debapriya Ghosh, 83, died the following day. |
| Inquest Findings | Both deaths were deemed accidental but were significantly affected by neglect and lack of supervision. |
| Circumstances of Falls | Ward fell due to inadequate nursing care after being admitted for frailty; Ghosh fell while unmonitored after waiting in the corridor. |
| Causes of Deaths | Ward’s death linked to risk factors not addressed; Ghosh’s death was avoidable with proper supervision. |
| Response from Hospital | St George’s Trust has launched immediate changes including increased staffing and fall assessments. |
| Coroner Comments | Senior Coroner Fiona Wilcox highlighted issues of demand in hospitals exceeding available resources. |
Summary
Hospital falls are a serious issue, as illustrated by the tragic cases of David Ward and Dr. Debapriya Ghosh, who both died after unwitnessed falls in an overstressed environment at St George’s Hospital. These incidents not only highlight the risks patients face due to inadequate supervision but also stress the urgent need for increased resources and reforms in hospital practices. Ensuring better staffing and vigilant patient monitoring is essential to prevent similar tragedies in the future.